Untangling Truths Navigating Mental Health with Ketamine Amidst the Opioid Crisis

Karina, a Multicultural Psychology Master's grad, excels in global project…
The opioid crisis has dominated discussions in the healthcare landscape, prompting exploration into alternative pain management solutions. Ketamine, a dissociative anesthetic, has emerged as a potential alternative, sparking debates about its classification and efficacy compared to opioids. In this blog, we will delve into the origins of ketamine, its mechanisms of action, therapeutic uses, and most importantly, debunk myths surrounding its classification as an opioid and will find out if is ketamine an opioid.
We will explore the role of ketamine in pain management and address a commonly asked question: How long does ketamine stay in your system? The opioid crisis has dominated discussions in the healthcare landscape, prompting exploration into alternative pain management solutions. Ketamine, a dissociative anesthetic, has emerged as a potential alternative, sparking debates about its classification and efficacy compared to opioids.
In this blog, we will delve into the origins of ketamine, its mechanisms of action, therapeutic uses, and most importantly, debunk myths surrounding its classification as an opioid and answer the crucial question: Is ketamine an opioid? We will explore the role of ketamine in pain management and address a commonly asked question: How long does ketamine stay in your system?
Understanding Ketamine:
Ketamine, distinct from opioids, operates by antagonizing the NMDA receptor. Approved by the FDA for anesthesia and pain management, ketamine boasts unique pharmacological effects. Administered in controlled settings, it has demonstrated success in mental health treatment, particularly for conditions like treatment-resistant depression and anxiety disorders. Research also supports its efficacy in chronic pain management, positioning ketamine as a promising alternative to traditional opioids.
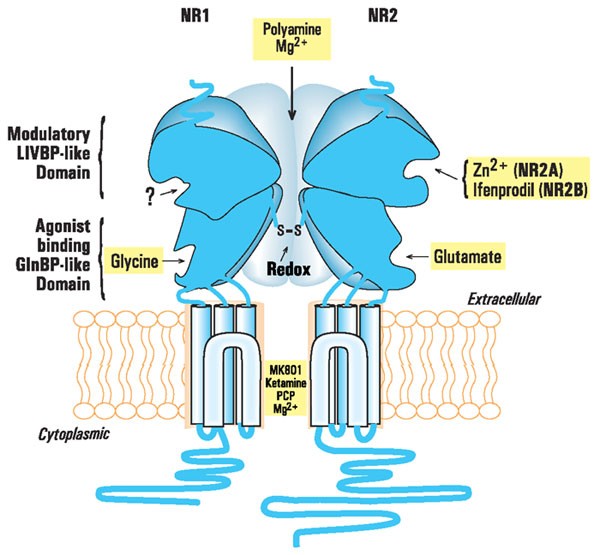
Credit: Nature Journal
Use of Ketamine:
The use of ketamine extends across various medical domains, demonstrating its versatility in addressing different conditions. Here are some notable applications of ketamine:
The Origin of Ketamine:
Synthesized in 1962 by chemist Calvin Stevens as a safer alternative to phencyclidine (PCP), ketamine initially found its place in surgeries. Despite its recreational use, ketamine’s therapeutic potential for mental health conditions, such as depression and bipolar disorder, has been extensively studied. Esketamine, a derivative, has gained FDA approval for treating treatment-resistant depression, emphasizing its evolution from a recreational substance to a valuable medical tool.
How Does Ketamine Work?
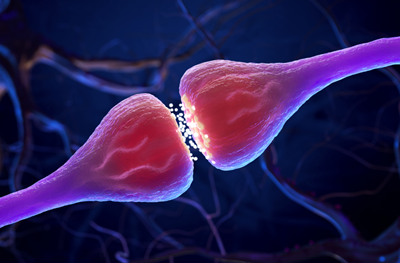
Ketamine’s mechanism involves inhibiting glutamate, a neurotransmitter, and activating opioid receptors for pain relief. Its antidepressant effects are linked to the mTOR kinase pathway, showcasing its versatility in addressing mental health conditions. Understanding these mechanisms is crucial for distinguishing ketamine from opioids.
The Opioid Crisis:

The opioid crisis, characterized by widespread misuse and addiction, has prompted a reevaluation of pain management strategies. Overprescribing of opioids has fueled addiction rates, resulting in severe health and social consequences. To address the crisis, alternative approaches like ketamine are being explored, with an emphasis on prevention, treatment, and harm reduction.
The escalation of the opioid crisis, particularly in the United States, is attributed to overprescribing practices. This has led to increased addiction rates and a shift to illicit opioids like heroin. The urgency to combat the crisis has prompted research into alternative pain management solutions, with ketamine emerging as a potential option.
Impact of Opioids on Health and Society:
Opioids, while effective for pain management, pose significant health risks, including addiction and side effects. The opioid crisis has strained healthcare systems, law enforcement, and public health resources. Recognizing the impact of opioids on health and society, there is a growing need for safer alternatives like ketamine.
Ketamine Vs Opioids:
Ketamine and opioids differ in their mechanisms of action and therapeutic effects. Ketamine’s success in treating chronic pain and depression, without the high risk of addiction associated with opioids, makes it a compelling alternative. Understanding these differences is vital for informed decision-making in healthcare.
Pharmacological Differences between Ketamine and Opioids:
Ketamine and opioids have distinct pharmacological differences, stemming from their mechanisms of action. While opioids target opioid receptors for pain relief, ketamine antagonizes the NMDA receptor. These differences underpin their varied therapeutic applications, reinforcing the need for a nuanced approach in clinical practice.
Both ketamine and opioids have therapeutic uses, but their applications differ. Ketamine, beyond anesthesia, proves effective in pain management and mental health treatment. Opioids, primarily prescribed for pain relief, carry a higher risk of addiction. Tailoring treatments based on these distinctions ensures optimal patient care.
Dispelling myths, ketamine is not classified as an opioid. Its distinct mechanisms and therapeutic applications challenge misconceptions, emphasizing the importance of accurate information for informed healthcare decisions.
Debunking Myths about Ketamine as an Opioid:
Despite scientific evidence, myths persist regarding ketamine’s classification as an opioid. Clarifying its unique mechanisms and efficacy in mental health treatment dispels misconceptions, paving the way for more informed discussions on pain management options. Robust scientific evidence refutes ketamine’s classification as an opioid. Clinical trials emphasize its effectiveness in pain management without opioid-associated side effects. Ketamine’s diverse therapeutic potential extends beyond the opioid crisis, reinforcing its distinct identity.
Is ketamine an opioid?
Ketamine is a dissociative anesthetic that primarily acts by antagonizing the NMDA (N-methyl-D-aspartate) receptor in the brain. It inhibits the activity of the neurotransmitter glutamate and also has effects on opioid receptors, contributing to its analgesic (pain-relieving) properties. Ketamine is often used for anesthesia, and pain management, and has shown promise in treating certain mental health conditions.
Opioids, on the other hand, are a class of drugs that include substances like morphine, oxycodone, and fentanyl. They work by binding to specific receptors in the brain known as opioid receptors, leading to pain relief and, in some cases, a feeling of euphoria. Opioids are commonly prescribed for pain management but come with a risk of dependence and addiction.
Attenuation of Antidepressant Effects of Ketamine by Opioid Receptor Antagonism
Antagonism refers to the opposing or inhibitory interaction between two substances, particularly in the context of pharmacology and physiology. In the case of ketamine, its mechanism of action involves the antagonism of the NMDA (N-methyl-D-aspartate) receptor. This means that ketamine blocks or inhibits the normal activity of the NMDA receptor, which plays a crucial role in the transmission of signals in the central nervous system.
The Role of Ketamine in Pain Management:
Ketamine’s role in pain management extends beyond its ability to provide relief. With its antidepressant effects and NMDA receptor antagonism, ketamine offers a safer alternative for opioid-resistant pain, potentially revolutionizing pain management strategies. Carefully administered ketamine infusions, even via nasal spray, provide targeted pain relief. Ketamine clinics follow stringent protocols for safe administration and symptom monitoring.
Ketamine’s unique mechanisms make it a valuable tool in addressing both physical and mental aspects of pain. Ketamine therapy presents a safer option for pain management, minimizing risks associated with opioids. Its dual benefits of pain relief and mental health improvement position it as a promising alternative, potentially transforming how chronic pain is approached in healthcare. The effects of ketamine last for a few hours due to its rapid metabolism and short half-life. Administered in controlled settings, the short duration ensures safe use and monitoring, addressing concerns about its presence in the body.
Conclusion:
In the evolving landscape of pain management, ketamine emerges as a distinctive and promising alternative to opioids. Its unique mechanisms, therapeutic versatility, and potential for improving mental health outcomes position it as a valuable tool in the healthcare arsenal. Dispelling myths and understanding the nuanced differences between ketamine and opioids are crucial steps toward informed decision-making, ensuring patient-centric and effective pain management strategies.
Karina, a Multicultural Psychology Master's grad, excels in global project management. A tech-savvy marketer and skilled podcaster, she empowers through wellness events. Passionate about diversity and innovation, Karina is a dynamic force in health and wellness.